You set off with a friend to do some hiking in the Rocky Mountains. Taking a red-eye out of New Orleans (7 feet/2.13 m below sea level), you arrive in Denver (5,431 feet/1,655.37 m above sea level), rent a car and, by mid-afternoon, you're driving up into the mountains, parking at a trailhead at 11,000 feet (3,352.8 m), hiking and finally setting up camp at 12,000 feet (3,657.6 m) above sea level.
The next day, you feel somewhat hungover. You have a headache and no appetite for breakfast. Your friend, on the other hand, feels great. The two of you continue ascending the mountain, gaining another 2,000 vertical feet (609.6 m) by nightfall.
Advertisement
That evening, you feel dizzy and nauseous and notice your feet are swollen. That night's rest is less than ideal -- you keep waking up with a start, rattled by the awareness that you stopped breathing in your sleep.
The following morning, your companion wants to continue, so you pay little heed to your reservations. While your friend is certainly no slouch, you're normally the faster, stronger and better-winded half of the duo. You can't help but wonder why you're feeling so poorly while your friend seems no worse for the wear.
You push on, but you can't seem to catch your breath -- even when you stop moving. After a labored day of climbing, the two of you camp at 14,000 feet (4,267.2 m). That night, you toss and turn in agony and feel like you're being suffocated. The following morning, you have a bad cough and tightness in your chest. By now, it's clear you have some sort of altitude sickness. Why did you -- and not your friend -- become ill? Was it preventable? Could you die?
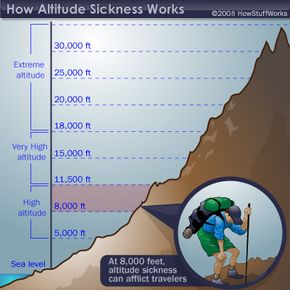
Altitude sickness can strike suddenly and unpredictably. And it's not just for the mountain climbers among us. Any rapid change in altitude can cause the onset of sickness. While most of our knowledge about altitude sickness is geared toward climbing (because the activity is based on rapid, steady rates of ascension) even flying or driving to higher altitudes can produce symptoms. For instance, flying into Peru at the airport in Cusco (elevation 11,000 feet above sea level) can cause you to feel the common effects of high altitude that day, but you'd naturally acclimate by staying at that elevation.
The sickness is largely a traveler's disease -- locals are acclimated to the elevation.
So how does altitude affect our bodies? We'll find out in the next section.
Advertisement